Total Hip Replacement
The introduction of total hip replacement surgery revolutionized people's ability to walk, function and really carry out near-normal function from a condition that was debilitating. Learn about the history of hip replacement surgery and what patients having total hip replacement surgery can expect.
Hosted by Eric Chehab, MD
Episode Transcript
Episode 1 - Total Hip Replacement
Dr. Eric Chehab:
Welcome to IBJI’s OrthoInform, where we talk all things ortho to help you move better, live better. I'm your host, Dr. Eric Chehab. With OrthoInform, our goal is to provide patients with a more in-depth resource regarding common orthopedic procedures that we perform every day. Today it's my pleasure to welcome Dr. Michael O'Rourke who will be speaking about all things total hip replacement. As a brief introduction, Dr. O’Rourke graduated with distinction from the University of Iowa in 1992. He received his medical degree from Loyola University here in Chicago. He returned to Iowa City for his residency training at the University of Iowa, known as one of the top orthopedic training programs– not just in the Midwest but in the entire country. Dr. O’Rourke completed his fellowship training at Rush University Medical Center where he worked with some of the godfathers of hip replacement surgery. Dr. O’Rourke began his practice at the University of Iowa before moving back to his home town here on the north shore of Chicago. He has helped thousands of patients with severe hip and knee disabilities. Dr. O’Rourke’s excellence has been recognized throughout his career including a prestigious AOA leadership award from the Kellogg School of Business. He was also recognized for his research as he was awarded the best fellowship research project in 2003. Dr. O’Rourke has published numerous academic articles regarding joint replacement. He has served as the head of the joint replacement center and is an outstanding surgeon and even better friend and colleague.
Mike, welcome to our inaugural OrthoInform podcast and thank you so much for taking the time to be with us.
Dr. Michael O'Rourke:
Thanks for having me.
Dr. Eric Chehab:
Just to begin, if you can give our audience a little bit of a background on the history of total hip replacement.
Dr. Michael O'Rourke:
Well hip replacements became more commonplace in the United States in the early seventies. The true godfather of hip replacements was Sir John Charnley from Wrightington, England. He really revolutionized the treatment of arthritis. There weren't really many successful treatments. The introduction of total hip replacements really revolutionized people's ability to walk, function and really carry out near normal function from a condition that was debilitating. Through the success of hip replacement - through the 1970s and the 80s - the fixation and techniques became more refined. When hip replacement started, the approach was a relatively traumatic approach where the muscles around the hip were cut off with a piece of bone and as techniques developed, approaches changed where less trauma was caused from the surgical approach. The implants became more versatile. There were more sizes, more fine tuning capabilities, improvements in fixation, the move from cemented hip replacements to in-growth hip replacements. And over the last couple decades there've been times through the history of hip replacements where there were maybe steps back and things were learned. And corrections have been made. And over the last couple decades it's been one of the most successful interventions we do in all of medicine.
Dr. Eric Chehab:
I'll tell patients that there's no better life preserving and quality-of-life restoring operation than the total hip. It's top of the list. You alluded to some of the advances in components when you're talking about a total hip replacement. What did it start with? It was just a plastic cup, some dental cement, and a metal stem initially. That's the Charnley hip replacement that you referred to. But now, take us through the current components of a hip replacement.
Dr. Michael O'Rourke:
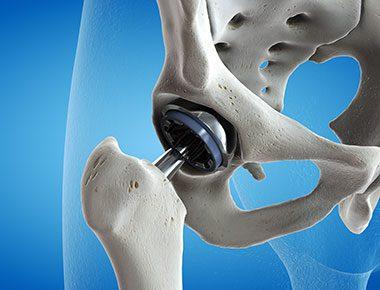
Well, a hip replacement is essentially a procedure where the femoral head- which is the round ball on the top of the thigh bone, is removed– and our bones as adults are filled with a fatty marrow. So on the stem on the ball side of the joint, there's a stem that is is anchored in the native femur and then that stem supports the ball that's used to replace the natural femoral head. On the socket side, which is part of the pelvis, there is a titanium shell that is a hemisphere essentially that's placed into the pelvis after the pelvis has been prepared to accept it.
The advances in those components have really been fixation and those were really in the eighties and nineties where press fit fixation - or fixation without the use of cement - became popularized and done. The shape and variety of the implants have improved to a to a state where we can achieve fixation relatively reliably with the implants we have. On both sides really the primary materials are titanium and occasionally there are other materials used on the stem side depending on the type of stem being used.
Dr. Eric Chehab:
So fixation is key and there have been significant advances in the fixation since the Charnley hip, correct?
Dr. Michael O'Rourke:
Yes.
Dr. Eric Chehab:
You mention also about the ball and in the pelvis side they’re bearings if I'm saying this correctly between the two components between the femoral ball and the acetabular socket. Tell us a little more about the bearings that are used in hip replacement.
Dr. Michael O'Rourke:
So hip replacements became successful with the use of a polyethylene insert that is placed on the socket side. On the ball side there are different materials used. Originally a stainless steel ball but more commonly an alloy of chrome cobalt and molybdenum alloy or a ceramic material. There are different bearings that have been used over the last ten to fifteen years with some hip designs which include a metal on metal hip replacement where rather than putting a plastic liner there's a metal liner or a one piece metal shell placed in the pelvis.
And that would be mated against a metal ball. There are ceramic on ceramic bearings and then there's mixes between the polyethylene on ceramic, polyethylene on metal, and ceramic on metal believe it or not. Those are some of the options that have been used. I would say that in today's environment, given some of the things we've learned, the most common bearing is a highly crosslinked polyethylene against either a ceramic head or a metal ball.
Dr. Eric Chehab:
The point of that bearing is to reduce the amount of wear is that correct? The wear particles can have a negative effect on the longevity of the hip replacement?
Dr. Michael O'Rourke:
Yes, so the bearing is the part that moves and it's the part that wears. Everything in life wears. There's always wear in all of these mechanical environments and the question is what happens to the wear particles. Wear is essentially small particles that are either sub micron or even smaller shed from a surface that's moving. It's the polyethylene that wears in a size that is typically managed by the body by a certain type of immune cell called macrophage. In those cells basically scavenger the particles. And In some bearing such as metal on metal there are there are smaller particles that can combine with proteins and activate a different type of immune cell that can respond to them. So some of the things we've learned over the last decade in particular are the potential negative impacts of of those metal on metal bearings which many of us have migrated away from.
Dr. Eric Chehab:
In our advances you mention a little bit we've had a couple of steps back but we've generally been progressing forward with hip replacement. it still remains one of the most incredible interventions that we have in all of medicine in restoring life for patients you mentioned a bit about the fixation on the bearing, is there a go-to that you use most of the time and they're exceptions that are made from there?
Dr. Michael O'Rourke:
There is a go-to that I use. I generally use a highly crosslinked polyethylene and a ceramic or ceramic like material for the head. There are other surgeons that will use a highly crosslinked polyethylene against metal head and there's very good data for that and nothing certainly wrong with that choice.
Dr. Eric Chehab:
In general, we're talking about patients who benefit from total hip surgery. Who’s your typical patient? Someone with arthritis? Or are there other conditions that also benefit from total hip replacement.
Dr. Michael O'Rourke:
The majority of patients are patients with osteoarthritis which is a loss of cartilage and bone rubbing bone and it causes stiffness and pain in a joint that leads to increased functional disability and pain. And the decision to do it is based on pain and function, not necessarily an x-ray. There are people that can live with arthritis and live pretty functional lives. And there are people who despite conservative treatment are doing poorly. That's when we decide to do it and that's and that's a majority of the patients that we do it for. There are other conditions such as avascular necrosis of the femoral head which is a blood flow problem to the ball which can lead to it can lead to pain and collapse of femoral head. That's a relatively common condition. There are post-traumatic conditions, femoral neck fractures - hip fractures. We’ll do total hip hips for more commonly nowadays than we previously did. That's the lion share of what we do it for.
Dr. Eric Chehab:
A patient undergoing total hip replacement - what can they typically expect as a result from their surgery?
Dr. Michael O'Rourke:
Well it's like I said earlier I mean it's a success story in medicine. And since the hip joint is a relatively simple joint mechanically and our fixation – our devices that we use to get fixation are reliable - we generally let people progress quickly in terms of weight bearing and function. There are different approaches to do hip replacement and most modern approaches spare trauma to the two muscles on the side of hip that are important to the function of the hip. And so people can recover quickly and start walking quickly towards not having a limp. So most patients use some form of assistive devices - either crutches or a walker for anywhere from you know days to a couple weeks and will transition to a cane .Again they’re weight bearing as tolerated and depending on the comorbidities of the patient or the patient's general conditioning before surgery there can be a big variety of how quickly people recover. If someone's really well conditioned and in good general health, they can oftentimes be on their feet without a cane in as quickly as a week or two. And other patients who are relatively deconditioned or have other issues such as spine issues will need assistance devices for a little bit longer. But usually I summarize to patients that you're eighty percent recovered at about four to six weeks, ninety percent recovered between eight and twelve weeks, and a hundred percent recovered in six months to twelve months.
Dr. Eric Chehab:
There are basically two standard approaches that are used within hip replacement - a posterior approach and anterior approach. Do you have any thoughts on the pros and cons of each approach?
Dr. Michael O'Rourke:
Yeah so when I did my training you know a lot of the advances in minimally invasive surgery were being performed and I had the privilege of working with a lot of people involved with that. When I started my practice, I started doing, you know, hip replacements with one of two approaches which was a mini posterior approach. And I also did an anterior approach where I spent some time after my training with the surgeon that helped popularize the direct anterior approach and so I did that for a couple years. And they're both friendly to the muscles on the side of the hip and I think people recover quickly with both of those approaches and there are pros and cons to both. I think both of those approaches are better tolerated than the most common approach to the hip replacement ten to fifteen years ago which would have been an anterolateral approach where a third to half of the muscle was taken off and repaired and recovery was a little extended under those circumstances.
Dr. Eric Chehab:
In terms of preparation, a patient coming into a total hip replacement; what are things that they can do ahead of time - or should do ahead of time? Physical therapy? Are they donating blood? Is there dental work to do? Colonoscopy? What are things that patients are expected to do that can help improve their outcome after total hip replacement?
Dr. Michael O'Rourke:
The general answer to that question would be to be in the most ideal shape they can be and given their other issues. You know, so physical therapy sometimes can be limited by the pain and physical limitations from the problems that we're addressing. Clearly trying to be in a routine of doing exercise can be very helpful and getting into that routine after surgery to help hasten the recovery. Being as healthy as you can be and optimizing your medical conditions beforehand are important. For diabetics, for example, having better glucose control before surgery can be important. Nutrition is often times overlooked, and making sure nutrition is optimized. Certainly there's a whole host of medical problems that the patient's internist is involved with clearing and involved in the clearing process to undergo surgery and optimizing those conditions from a standpoint of surgery it was very common to donate blood. It's become a much less common procedure – I would say a majority of surgeons across the country don't have patience donate blood routinely before surgery. In our experience has been the people have needed much less blood transfusion and go into the surgery with a higher hemoglobin which lets them recover a little faster. So most of us have gone away from our patients donating their own blood. Dental work is it's encouraged to have good dentition because poor dentition can lead to several medical problems including problems after any form of joint replacement. We’re putting implants that are expected to be there for thirty years in the body and we do some screening processes to make sure that patients who are carriers of bacteria on their skin or in their nasal cavity that we treat people to optimize their circumstances at the day of surgery.
Dr. Eric Chehab:
You mentioned thirty years - when a patient comes in I'm sure they ask “‘hey doc - how long do these last. How do you address that question? How long does it last? Sure, it's different depending on the health of the patient, the age of the patient, the activity of the patient. And so I'm sure there's not one answer for everybody. But in general what can patients expect in terms of longevity of a hip replacement?
Dr. Michael O'Rourke:
When you're making the decision do a hip replacement on the surgeons performing it, they’re making decisions with anticipation that this is going to be there for decades. Certainly whenever any surgical procedure is performed, there are always risks associated with surgical procedures and one of the risks with the joint replacement is the fact that it could need to be re done for various reasons. Either fixation problems, wear problems, or other unforeseen issues. In general, it's a probability question - meaning there's a certain percentage of people that are going to need a re-operation and at what time point. Most patients want to know, “what's my chance of going twenty years without needing another surgery?” For it to happen in general we have very good data and hip replacements looking at twenty year data and having survivorship data or success beyond twenty years ranging in the range of nine you know ninety percent of people going beyond twenty years with one operation. We have some data looking at a young group of patients with minimum thirty year follow up showing seventy percent survivorship in that age group you know thirty years after seventy percent of people still having their original hip replacement. So the anticipation is that we’ll get many decades. But you don't decide to do this unless you have a problem because you don't take any risk unless you need to.
Dr. Eric Chehab:
In terms of pain management, a lot of patients are somewhat afraid to approach joint replacement. They're worried about the pain that they may have with the procedure and immediately after the procedure. Do you mind just talking about what patients can expect in terms of pain management with a hip replacement?
Dr. Michael O'Rourke:
Since it's a relatively simple joint and the mechanics of what we are replacing it with are similar to the natural mechanics, you know it is a relatively well tolerated procedure with simple pain management. There are patients that don't need narcotic pain management certainly that can be a component of it. Most of the anesthetic techniques include some form of local infiltration of longer acting anesthetics which have helped in the early in the early phases occasionally we will do is...
Dr. Eric Chehab:
...These are relatively recent, aren't they? The longer acting anesthetics?
Dr. Michael O'Rourke:
Yeah within the last couple years they've been used more frequently. There's also regional anesthesia and regional pain procedures where there's a local anesthetic placed around regional nerves that can help immediate post-operative pain.
Dr. Eric Chehab:
Now that we've done so well with hip replacement we've begun to move it from something that required several days or weeks at the beginning in the hospital to something that could be done as an outpatient. Can you talk a little bit about the development of outpatient total hip replacements?
Dr. Michael O'Rourke:
Well I've been doing outpatient hip replacements for several several years now.
Dr. Eric Chehab:
When we say outpatient hip replacement we meaning basically same day procedure go home the same day is that.
Dr. Michael O'Rourke:
Yeah most people consider outpatient going home the day of surgery.
Dr. Eric Chehab:
Yeah.
Dr. Michael O'Rourke:
I think the time to discharges decreased dramatically from originally two weeks to on average under two days in the hospital for those who choose to stay in a hospital. And over the last two decades there's been a significant increase in the utilization of outpatient procedures for total hip replacements. Part of the reason for that is that hip replacements are a successful procedure where people feel so much better almost immediately after hip replacement. That over time we've just realize that it's it it's certainly as a doable thing doable thing and and probably more common than not moving forward.
Dr. Eric Chehab:
And likewise, as sort of a corollary to that, there seems to have been a big shift from patients going to a rehabilitation center for a week, two weeks, three weeks to going now directly home doing exceptionally well with that. what are some of the advantages of patients going directly home as opposed to some rehab center?
Dr. Michael O'Rourke:
Well many of us that do the procedure, and I've seen patients go through it, have long felt that going directly home from the location of where the surgery is done is the right thing to do. Going to skilled care facilities adds an additional level of exposure that that doesn't necessarily help the patients. For example, getting other communicable diseases - C. difficile, pneumonia and obviously in the era we're currently living in 2020 - COVID has really highlighted the importance of those concerns. So the disadvantages are just exposure to environments which could introduce something in the post-operative period that compromises either short term or or potentially long term results. The question is does more therapy help and and most of us don't think there's a direct correlation with more therapy being a beneficial thing. In fact, it may be that too much therapy in the early phases may be counterproductive. So I think it's very doable to go home. Most people are in a state where they're safe. And they get the appropriate amount of therapy in their home environment whether it be through home health, or as an outpatient to an outpatient physical therapy setting to have the optimal outcome.
Dr. Eric Chehab:
Again, it speaks to how far this operation has come, where patients were in the hospital for weeks on end, then in a skilled nursing facility for weeks on end, and now they're able to have the surgery one day, go home the same day, be very safe at home, have lots of resources for home, and essentially - not walk off the procedure but - walking off the procedure to some degree. That walking probably is one of the better forms of rehab that the total hip patient can have. You've outlined this and alluded to this: the first week after surgery, the first month after surgery, the first six months after surgery, about what it typically looks like. Can you just go over that ground again a little bit? That first week patients will most likely be using a cane or crutch for getting around, and then after a month will probably be walking independently or with a cane. You mentioned eighty percent of the recovery within the first four to six weeks, ninety percent within the first eight to ten weeks, yeah.
Dr. Eric Chehab:
Again it's a very predictable recovery.
Dr. Michael O'Rourke:
Yeah, and I think a lot of the variability comes from the baseline activity level and other medical comorbidities - depending on what their functional status was ahead of time. That has a big impact on their functional status and how quickly their functional status improves in the post-op period. So patients who are walking around generally get walking around very quickly. Patients who may be a little bit more frail and using crutches or a walker beforehand, or have a very very stiff hip for a period of time, it can take a little longer for those muscles to get strong again. Or for their other joints and comorbidities to adapt and build strength. So there's variability but most of that variability is related to the functional status beforehand.
Dr. Eric Chehab:
Okay and then just to talk briefly but importantly about some complications and pitfalls that can occur. What are some of the most common - though uncommon - complications that can occur with a total hip replacement?
Dr. Michael O'Rourke:
Again, it's a very successful surgery which has very low complication rate. The complications we get concerned about obviously as surgeons putting implants in, infection is one of the biggest things that we're concerned about. And we take every measure that we know how to take to minimize that risk in terms of and optimizing the patient's health ahead of time, using environments where the operation is done in the cleanest possible scenario, using pre-operative antibiotics, and doing an efficient surgery with teams of people who are very cognizant of all those issues. The rate of infection is extremely low. There's always a risk of dislocation with the hip replacement. The native hip rarely dislocates in any environment other than a major traumatic event. Hip replacements can dislocate no matter what approach is used to put them in. The rate of incidence of that is also very low and some of the modern materials and sizing options have really helped to reduce that risk.
Dr. Eric Chehab:
A hip replacement that's done today probably has a lower rate of dislocation than when that was done ten or fifteen years ago because of these changes in the components with the crosslinked polyethylene that you mentioned that greater size head that you can put in the correct–
Dr. Michael O'Rourke:
Yeah basically the improvement of the materials have allowed for choices to be made that mitigate that risk.
Dr. Eric Chehab:
So this has all been incredibly helpful, to take a journey through the history of hip replacement, some of the components of hip replacement, what patients can expect to prepare for hip replacement, what they can expect after their hip has been replaced. Is there anything else that you want to let a patient coming into a hip replacement know? Are there any pearls that you could share with us now? That would be terrific.
Dr. Michael O'Rourke:
I think most of the care of patients who have had problems is helping them navigate timing of doing it. I think when the indication is appropriate, expectations are usually exceeded - the patient's expectations are usually exceeded. Those expectations can be very high because it delivers on those high expectations and people are choosing it earlier in the disease process than they previously did. I think we're in a very good era of hip replacements because we've had some issues in the past with different bearings that I alluded to earlier where the country and the world of hip replacement have learned a lot of important lessons. And the materials that are being used now are quite good and have very good track records. And so I think it's a very good era of hip replacements. And in terms of the decision to do it I think it's really a personal decision that needs to be worked out with the surgeon and that that trust has to be there because it's a long-term relationship a surgeon has with the patient when they embark on this. Most of us see our patients for the rest of our careers. There's a relationship and a follow-up that happens at sometimes every five years sometimes a little bit more frequently than that so I think having that relationships is a really important component.
Dr. Eric Chehab:
Well I can say this because I see it. During the holidays in particular, the stack of boxes of chocolates that patients bring you and the bottles of wine and champagne and gifts because, almost all the time, you are exceeding their expectations. You deliver on an operation that changes their lives. They are so grateful. They are some of the most grateful patients that come into any practice who have their hip done, particularly by you. So I wanted to thank you very much for taking part in the inaugural OrthoInform podcast. Thank you for being here.
Dr. Michael O’Rourke:
My pleasure, thanks for having me.
Don't Miss an Episode
Subscribe to our monthly patient newsletter to get notification of new podcast episodes.

